
While confirmation of bleeding and, if necessary, resuscitation of the patient is proceeding, the examiner should estimate the amount and rapidity of bleeding.

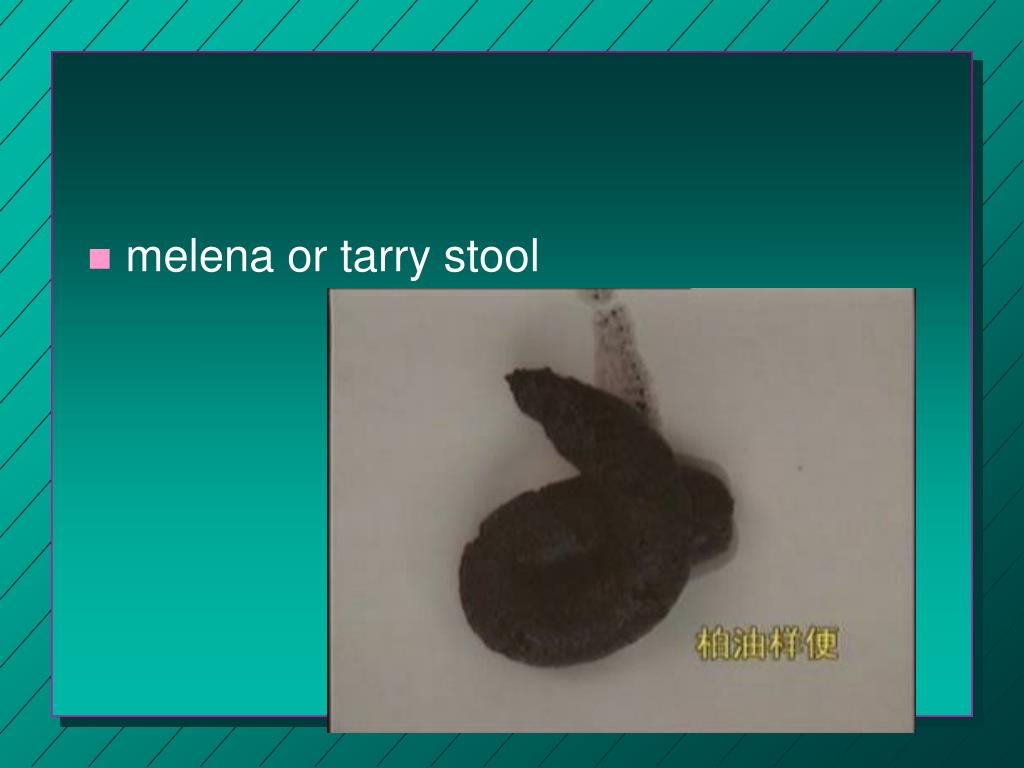
After asking about bowel habits, ask, "Have you observed blood in or on your stools or on the toilet paper?" and then, "Do you sometimes bleed from the rectum without passing stool?" It is important to follow with the direct question, "Have you ever had a black or bloody stool?" A similar sequence to elicit hematemesis might be: "Have you vomited during the past year?" If the answer is yes, ask, "What did it look like?" "Was it bloody?" "Was it brown, or did it look like coffee grounds?"ĭirect questions are the best approach to hematochezia. In this situation, to the extent allowed by the efficient use of time, open-ended questions, such as, "What are your bowel movements like?" or "Have you experienced a change in your bowel movements?" are preferable. The usual patient seeks a physician's help for reasons other than gastrointestinal bleeding. Nothing, however, should impede the immediate treatment of hypovolemia. If this brief history suggests acute bleeding, confirm the presence of bleeding through the testing of stool or gastric contents. Very rapid upper gastrointestinal hemorrhage, often from an arterial site in a peptic ulcer, may cause hematochezia. If slow intestinal transit occurs, melenic stools may be due to bleeding from sites as distal as the cecum. A melenic stool usually means upper gastrointestinal hemorrhage, whereas hematochezia usually has a colonic source.

Other substances, such as iron or bismuth, can turn the stool black. Melenic stools also have a stickiness that the patient often remembers. Make the patient understand that you mean jet black by comparing the stool color to a black object. The direct question, "Are your stools black or bloody?" should be used when active bleeding may be occurring. The patient with profuse epistaxis is almost invariably aware that a nosebleed has occurred. Hemoptysis is associated with coughing and is bright, foamy red in color. A careful history usually resolves this confusion. Occasionally hemoptysis or vomiting of swallowed blood from epistaxis can be confused with hematemesis. Hematemesis indicates that the bleeding is from the upper gastrointestinal tract, usually from the esophagus, stomach, or proximal duodenum. A bloody appearance is readily identified as hematemesis, but the coffee-ground appearance will not be recognized without direct questioning. The examiner should ask the patient if vomiting occurred, if blood or clots were present in the emesis, and if the vomitus looked brown, like coffee grounds, indicating the probable presence of blood. In the patient who may be bleeding profusely and need immediate treatment, directed rather than open-ended questions are appropriate. The patient having an acute gastrointestinal hemorrhage seeks a physician's help because of hematemesis, melena, or hematochezia, or because of symptoms of hypovolemia such as fainting or lightheadedness.


 0 kommentar(er)
0 kommentar(er)
